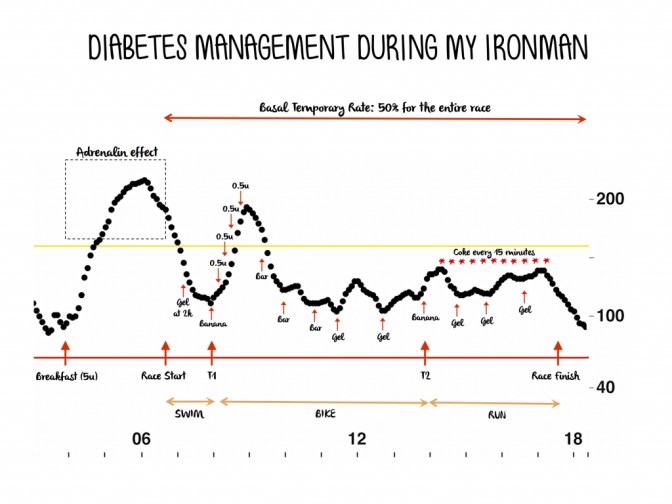
This page details my journey of developing a strategy to manage my blood glucose before, during, after activity and during races.
I will start with what I ended up using to complete Ironman Wales. It took me 15 hours to complete. My blood glucose stayed in range throughout the 1 hour 20 minute swim and 7 hour 35 minute bike ride. It went low during the run which tends to happens on my half Ironman distances too.
I ate my normal porridge and berries for breakfast. I ate cheese wraps cut in half on the bike. I also took 2 gels and 2 portions of bara brith during the ride. I had a chocolate bar to eat in transition before the run but I forgot to eat it because I was so excited and talking. (mistake number 1). I didn’t take food with me because I planned to take the flat coke and food from ironman feed stations (mistake number 2) and I had a cheese wrap in my special needs bag on the run.
My blood stayed in range for the first half of the marathon then it started to drop, not sure why but I didn’t pick up my cheese wrap from the special needs station (big mistake 3), I think just fatigued and not thinking straight. By my last lap (6.5 miles to go) the ironman feed stations ran out of food and coke they only had gels and red bull. I don’t take gels but I was now in a hypo so I took a couple and promptly vomited them back up! I took some red bull also. I made the decision to walk the last lap, I found an unopened SIS gel (the type I use) on the floor which I took and completed the ironman safely.
Post race I tried to eat some pizza but it made me feel sick so I had a cup of tea and a little water melon. My blood sugar returned back in range once I had finished the race surprisingly. I am not really sure what really happened during that last lap but my advice is to ALWAYS take food, be self sufficient!!
Glossary of Terms
Basal insulin is also known as background insulin it keeps blood glucose levels at consistent levels during periods of fasting. During fasting the body steadily releases glucose into the blood and insulin is needed to allow glucose into the cells to keep them supplied with energy.
Bolus insulin is taken at meal times to allow the uptake of glucose into the cells.
Hyperglycaemia (a hyper). This is when blood glucose levels are too high Hypoglycaemia (a hypo) This happens when your blood glucose level is too low, usually below 4 mmol/L.
Glycaemic Index The speed with which food can raise blood glucose levels
Low Glycaemic Index Foods give a slow rise in blood glucose
High Glycaemic Index Foods give a fast rise in blood glucose
What causes type 1 diabetes? https://www.diabetes.org.uk/type-1-diabetes
The cause of type 1 diabetes is still not known. It has nothing to do with diet or lifestyle.
About 8% of people with diabetes in the UK have type 1 diabetes. It’s a serious and lifelong condition. Over time, high blood sugar levels can damage your heart, eyes, feet and kidneys. These are known as the complications of diabetes. These can be prevented by managing your type 1 diabetes
Managing type 1 diabetes can be challenging.
Keeping your blood sugar levels within your target range
Carbohydrate counting
Eating a healthy diet
Exercising
Making healthy lifestyle choices
All this can make a difference to how you feel so you can live well with your condition and reduce your risk of developing complications in the future.
Further information NHS links :
https://www.nhs.uk/conditions/type-1-diabetes/
https://www.nhs.uk/conditions/type-1-diabetes/continuous-glucose-monitoring-cgms/
https://www.nhs.uk/conditions/type-1-diabetes/insulin-pumps/
History of my Diabetes Management
I have been lucky enough to be using the Omnipod insulin pump since 2018 and the Dexcom 6 continuous blood glucose monitoring since 2019. Both these have improved my diabetes management and reduced the amount of hypoglycemic events I was having. Before having these devises I had a lot of hypos so always ran a little high to try and avoid them. Beware they do go wrong on occasions just like any piece of equipment. They are only as good as your carbohydrate counting and carbohydrate to insulin ratios.
These devises have stopped me being scared that I was going to die in my sleep! I can also reduce my basal insulin before, during and after exercise which I find useful for preventing hypoglycemia. Thank you to my diabetes nurse and health care professionals that made this happen for me.
I still needed more help to manage my diabetes during exercise. I started most exercise sessions with high blood sugars (generally around 10 – 15 mmol or more) this is because I would lower my insulin bolus with the meal before, reduce my basal insulin just before and eat a snack before every session . This is what I had been advised to do to avoid hypos. Generally I felt sluggish at the start of most sessions because of the high blood glucose and then it would slowly lower and if it was longer session (more than 2 hours) I would dip into a hypo then back up high so enter a yo yo effect both during and after exercise.
I also wanted to eat less on the bike as I had gained weight. I started using High 5 powder in my water and dextrose tablets to try and stablise my blood sugar (straighten out my blood glucose line). These products have a definite carbohydrate content so it helps be more accurate with my carbohydrate counting.
1 dextrose tablet equals 3 g high glycaemic index (GI) or fast release carbohydrate

High 5 equals 44g fast release carbohydrate per 2 scoops which goes into 500ml water

Homemade Bara Brith equals 15g – 20 g of medium release carbohydrate per thin slice. I slice it up cover each individual slice in foil and put in the freezer ready to take out for bike rides.

Must have resource to count your carbohydrate accurately
2020 I managed to see a diabetes dietician who gave me so much information about managing my diabetes during exercise. This was the start of me taking control. I love strawberries, raspberries and blue berries but I had been avoiding them thinking they were high in sugar and quick release but I learnt they are really good medium release food so I eat them everyday with yoghurt for breakfast which fills me up and keep my blood glucose steady throughout the morning.
Exercising with Type One Diabetes (EXTOD) Conference http://www.extod.org
May and June of 2021 – I attended the extod education conference http://www.extod.org this has changed everything. I FEEL AWESOME WHEN I EXERCISE… well when I get it right, but I am learning to get it right more often!
First we learnt the different physiology between a diabetic athlete and none diabetic athlete. We were then introduced to think about the type, intensity, and regularity of exercise that we did and how this effects blood glucose.
Next we learnt how to stay safe before, during and after exercise
I learnt the action to take according to your blood glucose reading and trend before the start of an exercise session.
If my BG is 3.5 – 5-6 mmol I should take 20 g carbs
If my BG is 5.7 – 6.9 mmol I should take 15g carbs but if the trend is straight up no carbs are needed. If the trend line is straight down then twice the normal amount of carbs are needed at 20 minutes and 40 minutes during the exercise session
If my BG is 7 – 15 mmol then I should be good to go unless the trend line is straight down then I should take 15 g carbs
If my BG is greater than 15mmol I need to check my ketones and give a correction dose of insulin
If the trend is straight up
If I exercise around dinner time 6 pm I tend to have a snack a couple of hours before to stop me being hungry. I have no sugar peanut butter on one slice toast with no insulin. This equals 15g of carbohydrate and I find it does not raise my blood glucose above 10 before exercise. As well as filling my tummy it helps to give me a good starting blood glucose before exercise.
Next we learnt strategies to control blood glucose during exercise using the ICE agrononym. Insulin – Carbohydrate- Exercise
Insulin Adjustment
I learnt to think about how much insulin I have on board when exercising. Changes in my blood glucose happens slowly like the turning of a giant tanker, it takes time. This course has given me confidence and patience to know I have taken the correct steps to manage my blood glucose and to wait for the results. I do not panic so much and give myself too much insulin (results in massive hypos) or eat too much food (results in massive highs).
Before Breakfast Fasted Training
DISCOVERY from the EXTOD course before breakfast fasted training is the safest time to train because there is so little insulin onboard so reduces the risk of a hypo but does not eliminate the risk!
So the first time I tried this out I was not confident and did not trust the advice I was given, so instead I set my alarm for 1.5 hours before I was due to start exercise to reduce my basal by 50%. I went swimming and I did not have a hypo or take on any carbohydrate during exercise. However by blood glucose went very high after exercise. I did a similar thing a couple of times until I finally felt confident to just get up and go with no insulin reduction (which was the advice given from the course).
I did a 45 minute interval turbo bike ride with a starting blood glucose of 5.5 mmol and I had no hypo and no carbs were needed and I felt completely AWESOME LIKE A NORMAL NON DIABETIC PERSON. No stopping me now…… Next I ran, no hypo, then a turbo and a run then up to 1.5 hours of exercise, no hypos no highs!!! One morning I was little low so I took 10g of carbs before exercise 3 dextrose tablets. That worked well. I continue to exercise fasted with great success, but be warned you can still hypo. One morning after a night of drinking two large gins ( my limit) I had a hypo during my 10K fasted run. I finished the run with insulin turned off, 40g carbs and remained on hypo threshold.
Reducing basal insulin by 50% for exercise sessions
This is the big advantage of having the pump! Again 50% will not work for everyone it is a starting point and it also depends on your insulin trend, your previous activity , what you have eaten and how you feel before the exercise.
I find 50% insulin reduction works for my long bike rides, where I have generally eaten about 2 hours before and my blood glucose has reduced. If my blood glucose is above 10mmol I reduce my basal when the trend arrow turns down or lowers which happens typically 30 minutes into exercise session.
I generally reduce my basal between 30% – 50% just before sea swimming session.
The basal reduction for running varies the most . The effort or run type, the run distance, the time of day and my starting BG all influence.
Generally for short distance (30 minutes) tempo I will suspend insulin.
Hard efforts no reduction.
Endurance runs 50-80% reduction
Post Exercise Replace the Reduced Basal Insulin
I need to stop my basal reduction as soon as I stop exercise to reduce the risk of going high. Generally I find I need to replace some of the insulin I have missed during the basal reduction to prevent my blood glucose going high. I monitor this closely post exercise. If my blood glucose is low I will treat and monitor. I do generally eat with an hour of exercise too. If it is meal time I will have normal meal if not I will drink milk or have a slow release or protein snack.
Reduce bolus insulin by 50% if exercising within an hour of meal This works best for me if I exercise within 30 minutes as longer than this my blood glucose starts rising too high
Turning insulin off for exercise if its on downward trend, or unplanned exercise or I have given too much insulin at last bolus
This is an excellent emergency strategy to minimise the risk of a hypo. I use this if exercising the morning after alcohol consumption the night before.
When I have a hypo during exercise I stop, correct, wait (typically 5-10 minutes) then carry on… I used to treat the hyo and carry on exercising but recovery took longer and the session quality reduced.
Hypos can occur 12 hours after exercise. If I exercise in the evening I lower basal for a couple of hours by 20% when I go to bed to reduce risk of night time hypo.
Carbohydrate for exercise
The course has helped me calculate my EXcarbs (the carbohyrate I need during exercise). This is another strategy for managing diabetes during exercise, replacing the carbohydrate used. The EXcarbs are calculated by the exercise type, the intensity, length and your bodyweight. Below are my approximate EXcarbs. I weigh 63Kg
Swimming – 1.1g carbs per Kg body weight = approx 30g per hour
Cycling – 1.5 carbs per Kg body weight = approx 47g carbs per hour
Running – 1g carbs per Kg body weight = approx 30g per hour
Walking – 0.5 g carbs per Kg body weight = approx 15g per hour
I learnt the benefits of regular small snacks during exercise versus a large snack at the start of an exercise session. Information from the conference and experimentation has led me to use the following strategy for endurance bike rides – 50g carbohydrate per hour. (alternating every 20 minutes with 160ml high-5, 5 dextrose tablets or a thin slice Bara Brith). This works so much better for me than what I used to do having a sizeable snack before would give me high blood glucose for the start if exercise before dropping to low and then going on to cause a yo yo effect of highs and lows.
Exercise
If my blood glucose starts to reduce during exercise one option is to sprint for 10 seconds to give rise in BG for 20-30 minutes . I don’t tend to do this because at my age I don’t want to risk an injury.
Walking can lower blood glucose a couple of mmol if trying to reduce back into range. I use this method or slow running such as an extended warm up.
Carbohydrate During endurances Ironman Training 6 hours plus
I started to use cheese wraps with great success, the fat and protein kept my blood glucose steady. I still used High five, a little bara brith and occasional SIS gel.
Additional information from EXTOD conference
Here are some places where additional information can be
found.
Book
Diabetic Athlete’s Handbook by Sheri Colberg
Websites on exercise advice
http://www.extod.org
http://www.runsweet.com
http://www.teamnovonordisk.com
http://www.excarbs.com
Dietary advice
https://www.sportsdietitians.com.au/factsheets/dietsintolerances/
type-1-diabetes-and-exercise/
http://www.dafne.uk.com/
Interesting reads from Ironman with type one diabetes
Ironman Barcelona 2018 with Type 1 Diabetes!!!
My Race to the Finish Line: I’m an Ironman with Type 1
I have learnt that managing my blood glucose levels before and after exercise is just as important as during. Morning fasted exercise for short (up to 2 hours and steady) exercise reduces the risk of a hypoglycemic event because I have no bolus insulin on board. I also try not to inject bolus insulin within 3-4 hours of exercise as this also reduces the risk of a hypoglycemic event. Keeping an eye on my BG levels throughout the day and staying well hydrated I may reduce my basal insulin before exercise or eat a slow releasing snack suck peanut butter on wholegrain toast.
Please read on to the next page as I am now a qualified registered Dietitian and I now have a closed loop system